Researchers find acupuncture effective for the alleviation of tinnitus. This is significant given the intractability associated with this disorder. A research team in Sichuan, China, achieved significant positive patient outcomes by employing the use of electrical stimulation to acupuncture points. Compared with conventional manual acupuncture therapy, the addition of electroacupuncture to the treatment protocol increased clinical effectiveness for the treatment of tinnitus by 25.1%. Conventional manual acupuncture achieved a 64.5% total effective rate; however, electroacupuncture achieved an 89.6% total effective rate.
The Sichuan research team cited prior research and Traditional Chinese Medicine (TCM) theory as the basis for the development of their electroacupuncture clinical protocol. Zhang et al. identified acupuncture point Tinggong (SI19) as an important area for the treatment of tinnitus in prior research. The Sichuan researchers included SI19 in the study because the work of Zhang et al. finds SI19 effective for benefitting the ears, reducing tinnitus, improving conduction in the auditory nerves, and because electroacupuncture creates rhythmic contractions of the muscles in the region of the ear to promote circulation and subsequent delivery of nutrients to the hearing system.
The Sichuan researchers outlined the acupuncture procedure that achieved the clinical successes. In addition, they reviewed TCM diagnostic considerations for patients with tinnitus. In general, tinnitus is categorized as either excess type or deficiency type. Excess type is often exacerbated by anger, anxiety, and panic. This type is often related to liver and gallbladder inflammation that is either internal organ (Zang Fu) or acupuncture channel (Jing Luo) related. This diagnosis is referred to as liver fire and gallbladder excess that disturbs the ears by blocking the qi in the shaoyang meridian, in part, with damp-heat stagnation. Deficiency related tinnitus is often due to kidney or liver deficiency preventing nourishment from benefitting the ears. Diagnostically, this may be deficiency affecting the shaoyin and jueyin acupuncture channels.
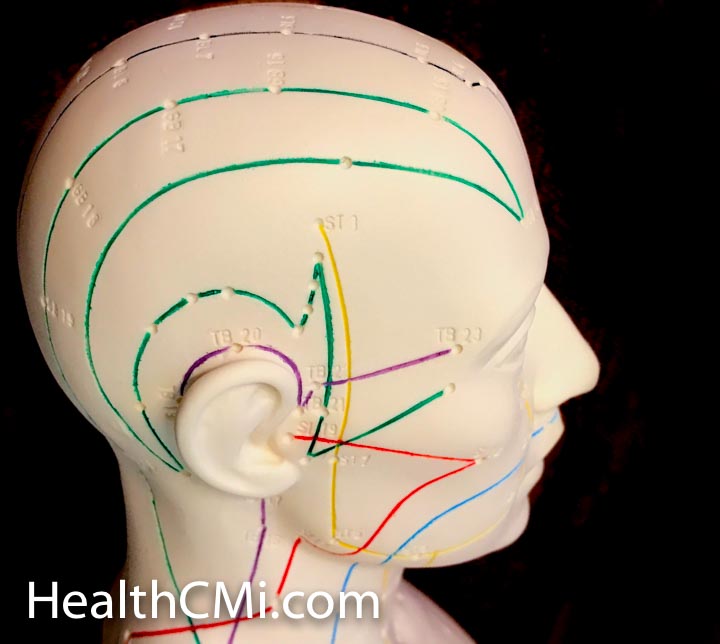
Two acupuncture treatment groups were compared in the clinical study. One group received electroacupuncture stimulation to the acupoints and the other groups received only manual acupuncture stimulation using reducing and reinforcing techniques. The primary acupoints used in the study were the following:
- Tinggong (SI19)
- Tinghui (GB2)
- Yifeng (TB17)
- Fengchi (GB20)
Secondary acupuncture points were added based on diagnostic considerations. For qi stagnation with blood stasis, Hegu (LI4) and Sanyinjiao (SP6) acupoints were added. For qi and blood deficiency, Qihai (CV6) and Zusanli (ST36) were added. For hyperactivity of liver and gallbladder fire, Taichong (LR3) and Qiuxu (GB40) were added. For kidney qi deficiency, Taixi (KD3) and Guanyuan (CV4) were added. For insufficient kidney qi and yang, Shenshu (BL23) and Mingmen (GV4) were added. For hyperactivity in the channels affecting the liver, Zhongzhu (TB3) and Waiguan (TB5) were added.
After acupoint site disinfection, filiform acupuncture needles were perpendicularly inserted. For excess syndrome, reducing (xie) techniques were applied. For deficiency syndrome, reinforcing (bu) techniques were applied. The deqi response was directed toward eliciting sensations towards the ears. Upon arrival of deqi, Tinghui (GB2) and Yifeng (TE17) were connected to a model G-6805 electroacupuncture device. A continuous wave was set to intensity levels at patient tolerance levels. This was achieved by starting at a very low intensity level of stimulation and slowly raising the amperage. The duration of electrical stimulation was 30 minutes.
Treatment was applied once per day for 15 days to complete one course of care. A total of 2 – 3 courses of care were applied. Using this protocol, manual acupuncture achieved a 64.5% total effective rate and electroacupuncture achieved an 89.6% total effective rate.
Researchers from the Central Hospital of Otolaryngology and Head and Neck Surgery in Chaoyang City achieved an 80% total effective rate using a different protocol. They used the following acupoints for the treatment of tinnitus:
- Yiming (extra)
- Tianyou (SJ16)
- Fengchi (GB20)
- Wangu (GB12)
- Tinggong (SI19)
- Shangyang (LI1)
- Kunlun (BL60)
- Juegu (GB39)
- Ashi
- Zhongzhu (KD15)
In a related study, Song et al. achieved significant clinical results for the treatment of tinnitus. Perhaps the most important aspect of the study by Song et al. is that the patient inclusion criteria sorted for intractable tinnitus. Only pernicious cases of tinnitus were admitted to the study.
Exclusion criteria sorted for cervical dysfunctions and ear deformities. Also excluded were patients with head injuries, anemia, diabetes, hypothyroidism, hypoglycemia, and autoimmune diseases. All patient admitted to the study had tinnitus for at least 4 months and up to 11 years. The total effective rate was 91% using the following set of acupoints:
- TB17 (Yifeng)
- GB2 (Tinghui)
- SJ21 (Ermen)
- SI19 (Tinggong)
- SJ3 (Zhongzhu)
- LR3 (Taichong)
- GB40 (Qiuxu)
- LU7 (Lieque)
- GB43 (Xiaxi)
Acupuncture points TB17, GB2, and SJ21 were unilaterally applied to the affected side, where applicable. If the tinnitus was unilateral, the patient rested on their side during the treatment. For bilateral tinnitus, patients rested in a supine position. Manual acupuncture stimulation was applied to bring about the arrival of deqi. Similar to the earlier study mentioned in this article, electroacupuncture was applied to local ear acupoints using a continuous wave. Total needle retention time was 30 minutes. Acupuncture treatments were administered once per day for a total of ten days.
Ginger moxibustion was applied. Ginger was sliced into 1 cm thick cubes, each with a tiny needle punctured hole in the center. Moxa was placed on the ginger and ignited. The ginger was placed on the outer auricle region to warm the area.
The statistics demonstrate important patient outcomes: 64.17% of all patients fully recovered, 14.71% had significant improvements, 11.76% had slight improvements, 8.82% had no improvements. The total effective rate was 91.18%. The researchers concluded that manual acupuncture combined with electroacupuncture and ginger moxibustion is effective for the treatment of intractable tinnitus.
References:
Zhao Y & Xie XY. (2013). Treatment Efficiency Observation of Electro-acupuncture for 48 Cases of Nervous Tinnitus. Chinese Manipulation & Rehabilitation Medicine. 4(4).
Zhang XT, Yuan GL, Xu M, et al. (2002). The effects of acupuncture on inner Tinggong acupoint to brainstem evoked potentials on patients with sudden deafness. Journal of TCM. 43:68.
Montazem A. Secondary tinnitus as a symptom of instability of the upper cervical spine: operative management. Int Tinnitus J. 2000;6(2):130–133.
Shore S, Zhou J, Koehler S. Neural mechanisms underlying somatic tinnitus. Progress in brain research. 2007 Dec 31;166:107-548. University of Michigan, Ann Arbor, MI.
Xue H. (2015). Treatments of cervical tinnitus between neck acupoints acupuncture and traditional acupuncture. Jilin Journal of Traditional Chinese Medicine. 35(9).
Adams PF, Hendershot GE. (1999). Current estimates from the National Health Interview Survey, 1996. Vital Health Star10. 200: 81-103.
Zhu Y. (2005). Tinnitus epidemiological investigation in Northern Shaanxi. Journal of Disease Control. 12(6): 149-150.
Yingli Song, Li, Shilin, Yan Xiao, and Jiang Wu. “Efficacy Observation of Acupuncture Combined with Ginger Moxibustion to Treatment of 34 Cases of Intractable Tinnitus.” Zhongyi Zhongyao (Traditional Chinese Medicine and Herbs) Aug. 2013: 277-278.